What Causes Keloid Scars and How Are They Treated
- Adam Burling
- Oct 15, 2025
- 13 min read
Keloid scars are a tricky business. They’re what happens when the skin’s healing process goes into overdrive, thanks to an overproduction of collagen. Instead of the body neatly patching up a wound and calling it a day, it keeps building scar tissue. This causes the scar to grow far beyond the original injury's boundaries, a process that's heavily influenced by our genes.
A Deeper Look at Keloid Formation
Have you ever noticed a scar that didn’t just heal flat but continued to grow, becoming raised, firm, and larger than the initial wound? You might be looking at a keloid. Understanding what causes keloid scars is the first step toward managing them effectively, a common concern for many of our patients here at Mid-County Dermatology in St. Louis.
Unlike typical hypertrophic scars that politely stay within the original wound area, keloids have a mind of their own, expanding into the surrounding healthy skin. The process can start with something as simple as a surgical cut, a piercing, or even a bad acne blemish. At Mid-County Dermatology, our board-certified St. Louis dermatologists, Dr. Feigenbaum and Dr. Gibstine, often explain it as the body’s healing mechanism getting stuck in the “on” position.
The Overzealous Healing Response
Think of your body's healing cells, called fibroblasts, as tiny construction workers. Their job is to rebuild damaged skin using collagen as their primary material. In a normal healing process, these workers get a clear signal to stop once the repair is complete.
But for people prone to keloids, that signal never arrives. The fibroblasts just keep going.
Excess Collagen: They continue pumping out collagen long after the wound has closed up.
Disorganized Fibers: This new collagen isn't laid down in a neat, orderly fashion. Instead, it's thick, jumbled, and disorganized.
Continuous Growth: The result is a scar that can keep growing for months or even years, creating that characteristic keloid appearance.
This simple infographic below illustrates the three key stages of keloid formation perfectly.
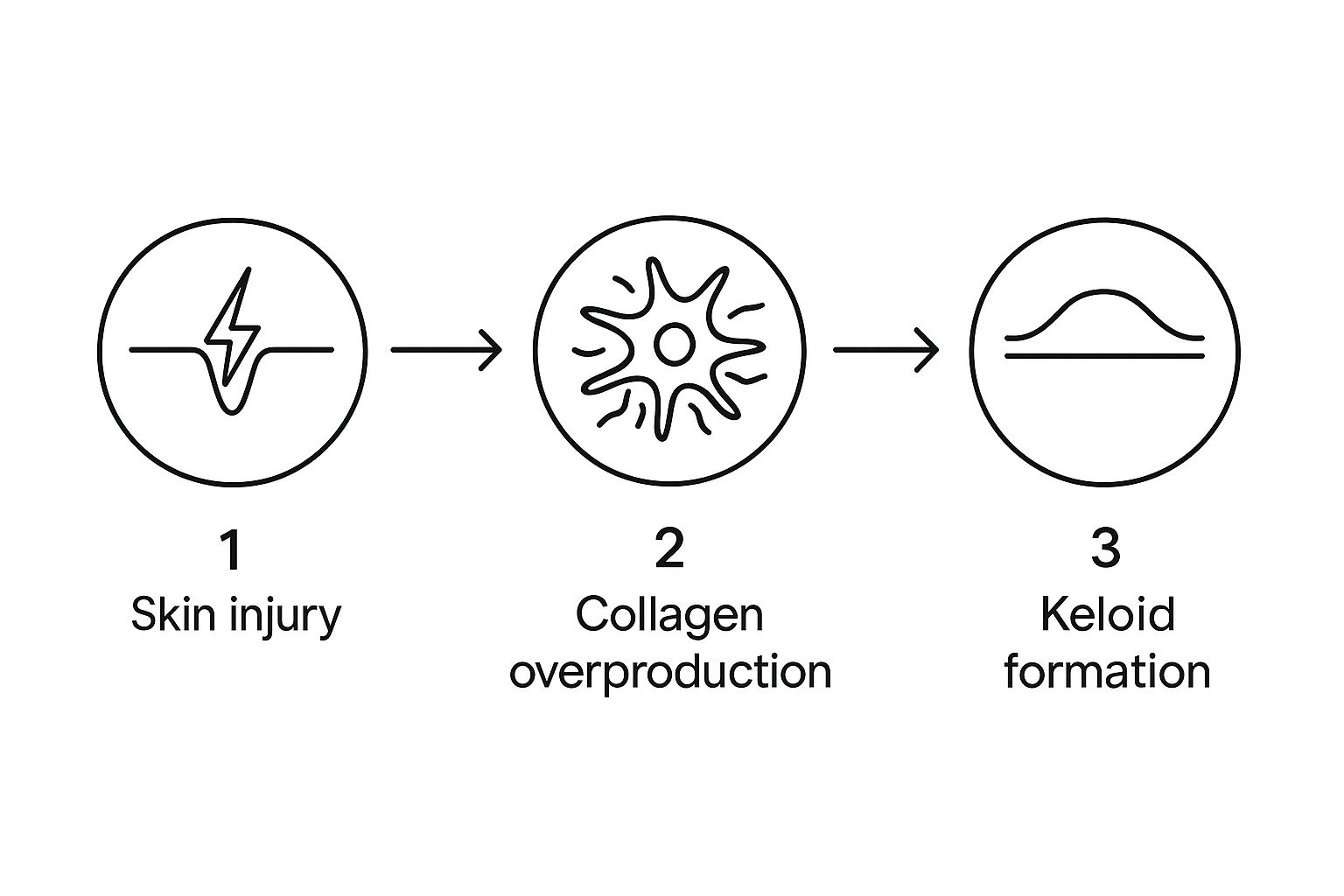
As you can see, a straightforward skin injury triggers an out-of-control collagen response, which leads directly to that raised, overgrown scar.
To help you get a quick handle on this, here's a summary table breaking down the essential factors.
Keloid Scars At a Glance
Factor | Description |
|---|---|
Primary Cause | An excessive, uncontrolled production of collagen by fibroblast cells during the healing process. |
Key Difference | Unlike hypertrophic scars, keloids grow beyond the boundaries of the original wound. |
Genetic Link | A strong genetic predisposition exists, especially in individuals with darker skin tones. |
Common Triggers | Surgical incisions, acne, piercings, burns, and even minor scratches can trigger keloid formation. |
High-Risk Areas | The chest, shoulders, back, and earlobes are particularly prone to developing keloids. |
This table provides a snapshot of why keloids form and who is most at risk. It’s a combination of how your body is wired and what kind of trauma your skin experiences.
If you live in the St. Louis area, from Clayton to Creve Coeur, and are concerned about a scar that won’t stop growing, our team of skin specialists can provide a clear diagnosis and a personalized care plan. Our St. Louis dermatology experts are here to help you understand your skin and find the right solution.
The Biology Behind Keloid Formation
To get a handle on what causes keloid scars, we first have to look at how skin normally heals—and then pinpoint exactly where that process goes haywire. When you get any kind of injury, your skin kicks off a brilliant three-stage repair mission to close the wound and rebuild. A keloid is what happens when this carefully orchestrated process gets completely derailed.
Normally, healing unfolds in a neat, controlled sequence. It starts with inflammation to fight off infection, moves to proliferation to create new tissue, and finishes with remodeling to strengthen and finalize the repair. Think of your skin's fibroblasts as diligent little construction workers. Their main job is to produce collagen, the protein that acts like scaffolding to rebuild the damaged area.
Where Normal Healing Goes Wrong
In a typical healing scenario, once the wound is closed, a signal tells the fibroblasts to pack it in and stop producing collagen. The construction phase is over. The scar then gradually flattens and softens over time.
But with keloids, that "stop" signal is either ignored or maybe never even sent.
The fibroblasts just keep working overtime, churning out far more collagen than is needed. It’s not just a quantity issue, either; the quality of this collagen is different. Instead of neat, organized fibers that support the skin, the collagen in a keloid is thick, dense, and chaotically jumbled, which creates that classic raised, tough texture. This is a key reason why patients from Ladue to Chesterfield seek a St. Louis skin specialist for treatment.
"A keloid is essentially a scar that doesn't know when to stop growing. Its cellular machinery for repair remains switched on, causing it to expand well beyond the original injury site."
This runaway production explains how something as minor as an ear piercing or a single acne spot can mushroom into a large, prominent scar. The initial injury is just the trigger for a massive biological overreaction lurking underneath.
The Role of Cellular Signals
The root of the problem lies in the complex communication network between your skin cells. Several growth factors and signaling pathways are in charge of keeping the healing process in check. In people who are prone to keloids, this system is seriously out of balance.
Here’s a look at the main players:
Transforming Growth Factor-Beta (TGF-β): This is a key protein that acts like a foreman, telling fibroblasts to produce collagen. In keloid-prone skin, its activity is abnormally high and stays elevated for far too long.
Fibroblast Overactivity: The fibroblasts themselves seem to be extra sensitive to these growth signals. They react more strongly and produce collagen at a much higher rate than they should.
This cellular hyperactivity is why keloid formation can continue for months or even years after the initial injury is long gone. At Mid-County Dermatology, Dr. Feigenbaum and Dr. Gibstine often explain that many advanced treatments are designed to interrupt these specific cellular signals to finally halt the scar’s growth.
Understanding Genetic and Racial Risk Factors
While any injury to the skin can leave a scar, not everyone develops keloids. The biggest clue as to why often lies in your family tree. If a parent or another close relative has keloids, your own risk shoots up significantly, pointing to a strong genetic link passed down through generations.

This genetic connection is the primary reason some people form keloids after a minor scratch, while others can have major surgery and never see one. At Mid-County Dermatology, our St. Louis dermatologists, Dr. Feigenbaum and Dr. Gibstine, always consider family history a key part of their diagnosis and treatment planning for patients from Ladue to Frontenac.
The Impact of Skin Pigmentation
One of the most well-documented factors in keloid formation is skin pigmentation. Study after study confirms that people with darker skin tones—including those of African, Hispanic, and Asian descent—have a much higher chance of developing keloids.
This isn't due to any sort of flaw in the skin. Instead, it's a direct result of genetic traits tied to melanin production and how fibroblast cells behave. In fact, people with darker skin are estimated to be 15 to 20 times more likely to form keloids than people with lighter skin.
Understanding this predisposition is crucial for providing effective and culturally sensitive care. A St. Louis skin doctor must recognize that a patient's genetic background is a vital piece of their overall skin health profile.
This heightened risk is clearly reflected in global numbers. According to research published in Skin Appendage Disorders (2024), the prevalence of keloids in England is estimated to be as low as 0.09%. That number jumps dramatically to around 8.5% in Kenya and reaches as high as 16% in Zaire. The most affected age group tends to be younger people between 10 and 30 years old. You can read the full research about these keloid prevalence findings for a deeper dive into the data.
Why Genetics Matter So Much
Think of your DNA as the instruction manual for how your body works. For people prone to keloids, that manual has specific instructions that can trigger an overactive healing response. Scientists have even started to pinpoint several genes believed to play a role in keloid development.
These genetic factors can influence:
Fibroblast Activity: Genes can make fibroblast cells inherently more aggressive in producing collagen.
Growth Factor Regulation: Your genetic code might not properly regulate the "stop" signals for healing, like TGF-β.
Inflammatory Response: A person's genetics can also dictate the intensity of their inflammatory response to an injury, creating the perfect environment for a keloid to grow.
This genetic foundation explains why keloids often run in families and are more common in certain populations. It’s a biological reality, not a lifestyle choice. At Mid-County Dermatology, we serve a diverse community across St. Louis, from Creve Coeur to Chesterfield, and are dedicated to providing expert care that acknowledges and respects these important genetic differences.
Common Triggers That Can Lead to Keloids
While your genes might load the gun for a keloid to form, it's almost always a specific skin injury that pulls the trigger. For people who are predisposed, a whole range of common skin traumas can kickstart that over-the-top healing response. Understanding these triggers is a huge part of prevention, a strategy we talk through with patients all the time at our St. Louis dermatology practice.

It's surprising, but even small, seemingly minor injuries can be enough to get a keloid started. The size or depth of the wound isn't always what matters most. It’s all about how your body's unique healing programming responds to any damage. This explains why one person might get a keloid from something another person heals from without a second thought.
High-Tension and High-Trauma Injuries
Some types of wounds are just riskier. Why? Because they put significant tension and trauma on the skin. This prolonged stress can keep the cellular "on" switch for healing flipped for way too long, basically telling the fibroblasts to just keep pumping out collagen.
Common high-risk triggers include:
Surgical Incisions: Any surgery is a risk, but areas where the skin is naturally tight—like the chest, back, and shoulders—are particularly vulnerable.
Deep Lacerations or Cuts: Any injury that gets down into the deeper layers of the skin can set the perfect stage for a keloid.
Burns: Both heat and chemical burns cause such extensive tissue damage that they often lead to abnormal, overgrown scarring.
Seemingly Minor Skin Injuries
This is the part that often surprises people. You have to realize that even minimal skin trauma can lead to a very significant keloid in susceptible individuals. At our clinic, we often see patients who are shocked that a tiny injury resulted in such a large, growing scar.
"A keloid doesn't require a major injury. For someone with the genetic tendency, something as simple as an insect bite, a piercing, or an acne pimple can be the starting point for a scar that grows for years."
Other everyday triggers can include:
Ear and Body Piercings: Earlobes and cartilage are classic hot spots for keloid development.
Tattoos: Think about it—the repeated needle punctures from tattooing create thousands of tiny micro-wounds.
Vaccination Sites: An injection, like a flu shot, can sometimes trigger a keloid on the upper arm.
Scratches or Abrasions: Yes, even a simple scrape can be enough to start the process.
The Role of Chronic Inflammation
Constant, low-grade inflammation is another major player in causing keloid scars. When the skin is always irritated and trying to repair itself, it creates the perfect storm for the healing process to go haywire. This is a big reason why managing underlying inflammatory skin conditions is so critical.
Conditions like atopic dermatitis (eczema) really ramp up the risk. In fact, a large-scale study published in Scientific Reports (2021) confirmed that patients with atopic dermatitis have a 3.19 times higher probability of developing keloids. The ongoing inflammation seems to put fibroblast activity into overdrive during any wound healing. You can read the full research about the link between atopic dermatitis and keloids to learn more.
Similarly, severe inflammatory acne—especially cystic acne—is a well-known trigger. Each inflamed cyst is essentially a deep wound that can heal with a keloid, particularly on the chest, back, and jawline. If you're dealing with painful bumps under your skin, getting a proper diagnosis is crucial, and you can learn more about different types of cysts in our detailed guide. Effectively managing these conditions isn't just about having clear skin today; it's about preventing permanent scarring tomorrow.
Effective Strategies to Prevent Keloid Scars
If you know you’re prone to keloids—maybe they run in your family—prevention is your most powerful tool. You can't change your genes, of course. But you can control how you care for your skin after an injury, and that makes all the difference in heading off that overzealous healing response.
The entire goal is to create the perfect healing environment. You want to send signals to your skin that everything is calm, controlled, and healing just as it should.
Taking proactive steps after any skin injury, no matter how minor it seems, can have a huge impact. At Mid-County Dermatology, our board-certified St. Louis dermatologists, Dr. Feigenbaum and Dr. Gibstine, always stress to our patients in Clayton, Ladue, and the surrounding areas that consistent, early care is absolutely crucial.
Proactive Wound Care Techniques
Proper wound care is your first line of defense. The second you get a cut, scrape, or burn, it’s time to start treating it with care. This isn’t just about stopping an infection; it’s about minimizing inflammation to encourage a calm, controlled healing process.
Here are the essential steps to take right away:
Gentle Cleansing: Wash the area daily with mild soap and water. You want to remove bacteria and debris without irritating the delicate new tissue that’s trying to form.
Maintain Moisture: Keeping the wound moist is key. This helps prevent a hard, tight scab from forming, which can disrupt healing. A thin layer of an occlusive product like petrolatum creates a protective barrier that locks in moisture and promotes optimal repair. You can learn more about this simple but effective strategy in our guide on using petrolatum for skin care.
Protect from the Sun: Freshly healed skin is extremely sensitive to UV rays. Sun exposure can worsen inflammation and lead to darker discoloration, making the scar more noticeable. Keep it covered with clothing or a bandage, and once the skin has fully closed, use a broad-spectrum sunscreen diligently.
Advanced Prevention Methods
Beyond the basics, there are a few proven methods that can actively discourage a keloid from forming on a fresh wound. These techniques work by applying gentle pressure or creating a very specific micro-environment that helps regulate collagen production, telling it to slow down.
For anyone at high risk, we often recommend starting these preventive treatments as soon as the initial wound has healed over. The earlier you intervene, the better your chances of stopping a keloid before it even begins to grow.
Consider these options, which are often recommended by a St. Louis skin doctor:
Silicone Gel Sheets or Ointments: This is one of the most effective prevention strategies out there. Applying a silicone sheet or gel directly to a healing scar for 12 to 24 hours a day hydrates the tissue and is thought to down-regulate the cellular signals that tell your body to produce excess collagen.
Pressure Dressings or Garments: For larger wounds, especially after surgery on keloid-prone areas like the chest, applying continuous, steady pressure can physically restrict the scar from growing upward and outward. This is a very common practice after major incisions or burn treatments.
Finally, a bit of common sense goes a long way. If you know you're at high risk, it's wise to avoid elective skin procedures—like piercings or tattoos—in hotspots like the earlobes, shoulders, and chest. If you are considering one, having a conversation with a St. Louis dermatologist at Mid-County Dermatology first is an essential preventive step.
When to Consult a St. Louis Dermatologist
While many scars fade into memory, some demand a professional eye to manage correctly. If you spot a scar that seems to have a mind of its own and keeps growing, it's always a good idea to get it checked out. A sit-down with a qualified St. Louis skin specialist can give you a clear diagnosis and, more importantly, stop the scar from getting worse.
At Mid-County Dermatology, Dr. Feigenbaum and Dr. Gibstine help patients from Ladue to Frontenac make sense of their skin concerns. When it comes to keloids, jumping on treatment early is often the secret to getting the best results.
Key Signs to Watch For
It’s time to schedule an appointment with a dermatologist if your scar starts doing any of the following:
Grows Beyond Boundaries: The scar tissue is creeping past the original edges of the wound. This is a classic sign of a keloid.
Continues to Thicken: Months after the initial injury, the scar is still getting more raised, firm, or bulky.
Causes Discomfort: You're dealing with constant itching, tenderness, or even outright pain in the scar area. Scars shouldn't hurt long-term.
Affects Movement: The scar sits over a joint—like an elbow or knee—and has become so tight it's starting to restrict your range of motion.
It's also worth knowing that certain conditions can make you more prone to keloids. A large-scale analysis published in the Journal of Drugs in Dermatology (2024) found that a history of acne, atopic dermatitis, or rosacea can significantly bump up your chances of developing them. This makes getting a professional opinion even more critical.
You can read the full research about these keloid risk factors if you'd like to dive deeper. Learning how to find a trusted dermatologist in St. Louis is the perfect first step toward getting your skin back on track.
Your Keloid Questions, Answered
Here in St. Louis, we see a lot of patients who are understandably concerned about their keloid scars. It's a common topic, and a lot of misinformation is floating around. To clear things up, Dr. Feigenbaum and Dr. Gibstine at Mid-County Dermatology have put together answers to the questions we hear most often.
Will My Keloid Ever Go Away on Its Own?
This is a tough one, but the short answer is no. True keloids almost never disappear by themselves. While a different type of raised scar, called a hypertrophic scar, might flatten out over time, keloids are a whole different beast. They're caused by a healing process that just won't quit, so without treatment, they tend to stick around or even get bigger over the years.
I'm Worried My Keloid Is Cancerous. Is It?
It's completely natural to worry about any unusual skin growth, but we can set your mind at ease on this one. Keloids are completely benign, meaning they are not cancerous and pose no threat to your physical health. They are simply an overproduction of scar tissue.
That being said, it’s always smart to have any new or changing spot on your skin checked by a board-certified dermatologist. They can confirm the diagnosis and make sure nothing else is going on.
Do Keloid Injections Actually Work? Are They Painful?
Yes, corticosteroid injections are one of our go-to, first-line treatments for a reason—they are often highly effective. These injections get right to the source of the problem, calming the inflammation and telling the overactive cells to slow down collagen production, which is what makes the keloid grow in the first place.
At Mid-County Dermatology, we know the idea of an injection can be intimidating. You might feel a temporary sting or burning sensation, but we take every possible step to minimize discomfort. We want to make the procedure as comfortable as we can for all our patients, from Clayton to Chesterfield.
What's the Cost for Keloid Removal?
There’s no one-size-fits-all answer here, as the cost really depends on your specific situation. Several factors come into play:
The keloid's size and location on your body.
The type of treatment we decide on together (injections, laser therapy, surgical removal, etc.).
How many treatment sessions are needed to get the best result.
Your insurance coverage, since some plans may view certain treatments as cosmetic.
The best way to get a clear picture of the cost is to come in for a consultation. Our St. Louis skin specialists can walk you through all the options and provide an accurate estimate tailored just for you.
Ready to finally do something about your keloid scars? The board-certified dermatologists at Mid-County Dermatology are here to give you a professional diagnosis and a treatment plan that makes sense for you.
Schedule your consultation today and take the first step toward healthier, clearer skin.
This information is for educational purposes only and does not constitute medical advice. Please consult with Dr. Feigenbaum, Dr. Gibstine, or another qualified healthcare provider at Mid-County Dermatology for personalized treatment recommendations. Individual results may vary.
